
Claim Management
The quick + clear path to fuller reimbursement
For providers of all kinds, managing claims is one of the most demanding parts of the revenue cycle due to deep-rooted manual processes, a lack of visibility into payer data, and other challenges.
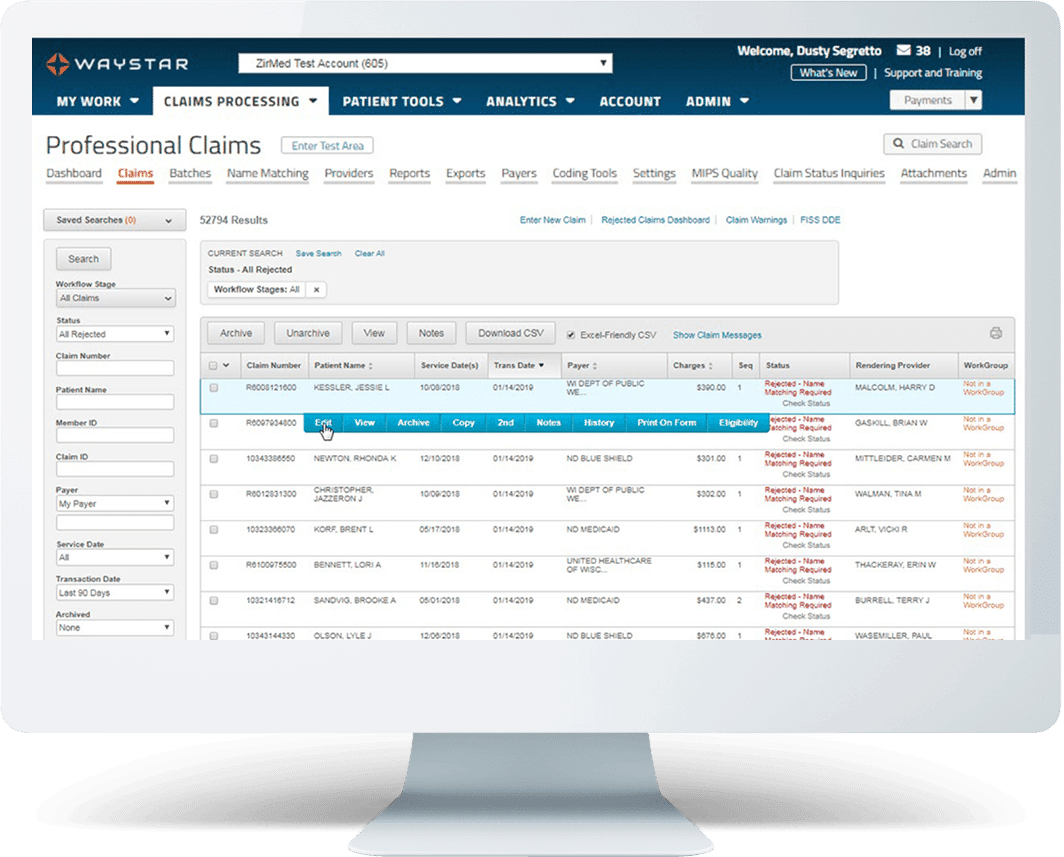
Things are different with Waystar. Our award-winning Claim Management suite can help your organization prevent rejections and denials before they happen, automate claim monitoring, and streamline attachments. What’s more, Waystar is the only platform that allows you to work both commercial and government claims in one place.
Request demo
Waystar Claim Management—by the numbers
“ Honestly, after working with other clearinghouses, Waystar is the best experience that I have ever had in terms of ease of use, being extremely intuitive, tons of tools to make the revenue cycle clean and tight, and fantastic help and support. ”
Explore our Claim Management solutions
Claim Manager | Claim Monitoring | Claim Attachments | Medicare Enterprise
Claim management resources
Take a deeper look at claim management
Below, we’ve compiled some tips and best practices surrounding claim management — and expert insights on how innovative technology can help your organization work smarter. Check out our resources below
A quicker path to more complete reimbursement
Claim status inquires: What’s at stake for your organization
Medical claims clearinghouse must-haves
Save time and money by filing claims electronically

Talk with a Waystar solution expert about Claim Management
Fill out the form below to have a Waystar expert get in touch. We look forward to speaking with you.